Introduction
Persistent Müllerian Duct Syndrome (PMDS), originally reported by Nilson in 1939, is an uncommon disorder affecting internal male sexual development. The condition may be idiopathic or inherited, most commonly through an autosomal recessive pattern (about 85%), but X-linked and autosomal dominant, sex-limited inheritance have also been described.1
It is an uncommon disorder of internal male pseudohermaphroditism in which Müllerian duct remnants are present in individuals with male genotype and phenotype. It results from mutations affecting anti-Müllerian hormone (MIS) or its receptor (MISR-II) and is inherited in an autosomal recessive manner.2,3
Development of the male external genitalia proceeds normally. However, regression of the Müllerian ducts does not occur, leading to persistence of the uterus, fallopian tubes, and the upper third of the vagina in individuals with a 46, XY karyotype. As a result, affected individuals have coexisting male and female internal reproductive structures.4
The aims of this case report are:
-
To raise awareness among healthcare professionals and highlight the pathophysiology, morphology, clinical features, and management of this rare entity.
-
To emphasize the unusual presentation of PMDS with hematuria and hemospermia, which may mimic menstruation.
Case Summary
A 48-year-old male from presented with a three-year history of recurrent hematuria and hemospermia. The episodes occurred several times per month and lasted for several days. He also complained of pushing-type lower abdominal pain, aggravated during sexual intercourse. He had no similar symptoms prior to three years ago.
The patient had visited multiple private hospitals and was treated repeatedly for urinary tract infection. Cystoscopy was performed without significant findings or improvement. Due to persistent symptoms, he presented to our hospital.
He had a normal sexual life and was the father of two daughters and one son. There was no family history of similar conditions. He denied inguinal swelling or other systemic complaints.
On physical examination, the patient was a tall, muscular man with well-developed secondary sexual characteristics. He had male-pattern baldness, moustache, beard, and normal axillary and pubic hair distribution. There was no gynecomastia. Systemic and abdominal examinations were unremarkable. Digital rectal examination revealed a normal-sized prostate.
The inguino-scrotal examination showed no inguinal mass or hernia, normal penoscrotal position, fully developed penis and scrotum, with both testes being normal in size and position
Routine laboratory investigations, including urinalysis, ECG, and chest X-ray, were normal.
An abdomino-pelvic ultrasound showed the urinary bladder being distended with normal wall thickness and no internal echoes. A bilobed oblong mass measuring 7.4 × 8.3 cm was seen on the right side, appearing to be connected to the bladder. The prostate was normal in size and echogenicity. These findings raised concerns for an incomplete bladder duplication.
A contrast-enhanced CT scan showed the right kidney to be located in the lower abdomen. A bicornuate uterus-like structure with a visible endometrial canal was identified, with the lower part connected to the prostate. The urinary bladder and prostate appeared normal. These findings were suggestive of male pseudo-hermaphroditism with right ectopic kidney.
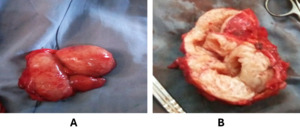
Patient was taken to the operating room, where an infra-umbilical midline vertical incision was performed. Intra-operatively, a bicornuate, pear-shaped structure with a tubular connection to the prostate (Figure 1), predominantly on the right posterolateral aspect of the urinary bladder, was identified. Surrounding structures were normal.
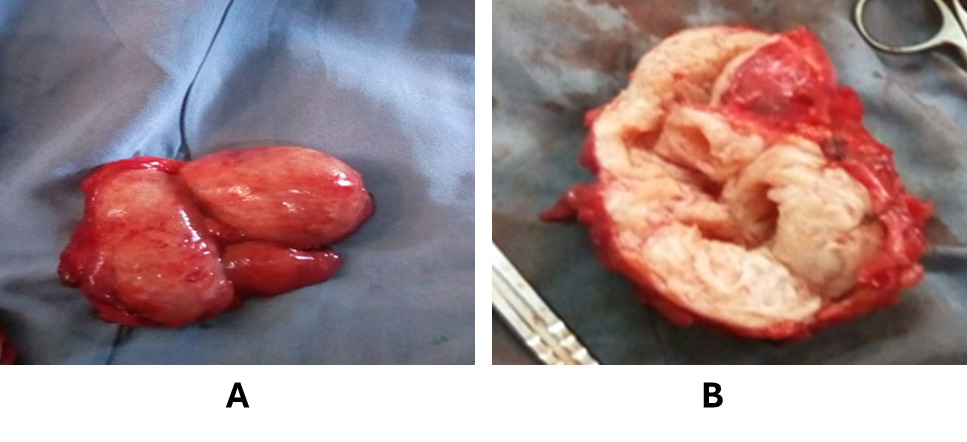
The structure was carefully dissected, the broad ligaments and blood supply were ligated, and the distal attachment to the prostate was double-ligated and excised. Hemostasis was secured, and the abdomen was closed in layers. Specimens were sent for histopathological examination.
The postoperative period was uneventful. The patient was discharged on postoperative day four. At the 2-week follow-up, he was asymptomatic, and histopathological examination revealed columnar-lined smooth muscle proliferation with endo-myometrial architecture, consistent with uterine tissue. No malignancy was detected.
At one-month follow-up, the patient remained asymptomatic with normal sexual function. Hormonal assays were within normal limits. He was followed for six months postoperatively with complete resolution of symptoms.
Discussion
Persistence of the Müllerian duct is a rare form of male pseudohermaphroditism characterized by the presence of Müllerian duct remnants in an otherwise male individual. People with PMDS exhibit a normal male phenotype and are therefore routinely assigned male sex at birth without any uncertainty. The condition arises from inadequate production of Müllerian inhibiting substance (MIS) or resistance of the target tissues to its action. PMDS is most often identified incidentally during surgical procedures for inguinal hernia or undescended testes, typically presenting as hernia uteri inguinalis.5,6
PMDS is typically inherited in an autosomal recessive pattern. Embryologically, both Müllerian and Wolffian ducts are present until the sixth week of gestation. In males, regression of Müllerian ducts is mediated by anti-Müllerian hormone (AMH) secreted by Sertoli cells.
PMDS results from either AMH deficiency (Type I), AMH receptor resistance (Type II), or idiopathic causes. Several genes, including AMH, WT1, SRY, SF-1, DAX-1, and SOX-9, have been implicated in abnormal sexual differentiation.
PMDS is categorized into three forms:
-
The female type (60–70%), characterized by bilateral intra-abdominal testes and epididymides attached to fallopian tubes in positions comparable to ovaries.
-
Hernia uteri inguinalis (20–30%), where one testis is located in the hernia sac or scrotum while the opposite testis remains intra-abdominal.
-
Transverse testicular ectopia (about 10%), in which both testes are found within the same hernia sac together with the uterus and fallopian tubes.7
Our patient had normally descended testes with preserved fertility, an extremely rare presentation. The periodic hematuria and hemospermia likely resulted from functional Müllerian remnants. Surgical excision was justified due to persistent symptoms and malignancy risk.
Conclusion
Although PMDS is rare, a high index of clinical suspicion is important due to its risk of malignancy and potential fertility implications. Imaging modalities such as ultrasound, CT, and MRI play a key role in diagnosis. Management is primarily surgical, with careful balancing of malignancy risk against fertility preservation.
Our patient showed complete symptom resolution postoperatively without complications. Approximately 11 cases of malignancy arising from retained Müllerian remnants have been reported, corresponding to a 3–8% risk.
Ethical Considerations
Written informed consent was obtained from the patient for publication. Ethical approval was obtained from the Arba Minch University Institutional Research Ethics Board (IRB No. IRB-23425/25).