Introduction
Subtotal cholecystectomy (SC) is typically performed for patients with complicated anatomy that prevents safe dissection of the cystic artery and cystic duct within Calot’s triangle.1 Significant inflammation, adhesions, and Mirizzi syndrome are all factors which may obstruct the view of Calot’s triangle and increase risk of bile duct injury. Subtotal cholecystectomies result in part of the gallbladder neck or posterior wall being left in place.2 Despite evacuation of stones within the gallbladder during cholecystectomy, the risk of cholelithiasis and cholecystitis is still present. We report a case of remnant cholecystitis treated by robotic-assisted laparoscopic cholecystectomy.
Case Description
Patient is a 39-year-old male with a past medical history of remnant symptomatic cholelithiasis status-post subtotal laparoscopic cholecystectomy. He presented to the emergency room with one day of right upper quadrant (RUQ) abdominal pain which began that morning and progressively worsened accompanied by nausea and decreased oral intake tolerance. He was afebrile and denied any vomiting. Upon physical examination he was negative for Murphy’s sign but was moderately tender to epigastric and RUQ palpation. Complete blood count was normal aside from a high lymphocyte and low neutrophil count, potentially indicative of inflammation.
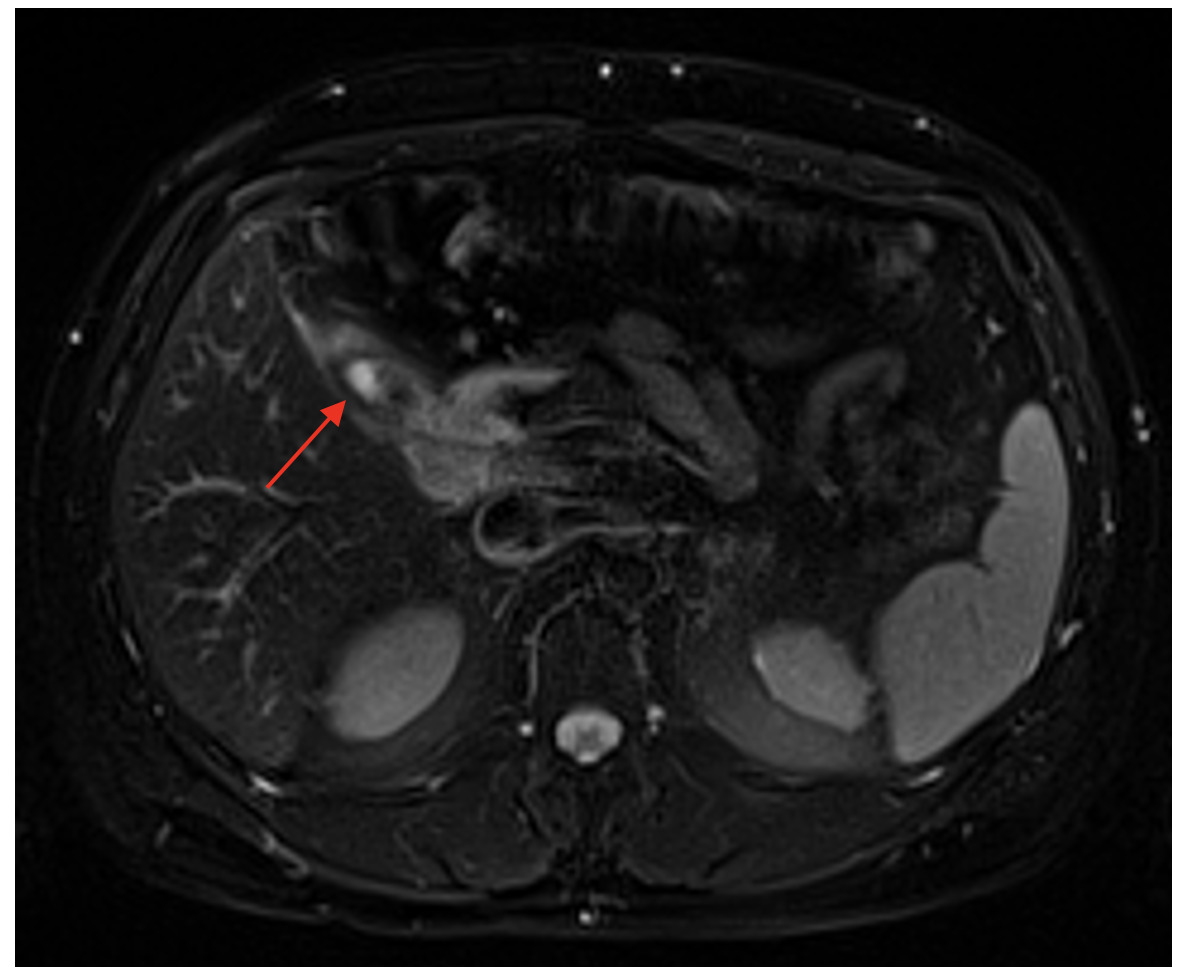
Initial computed tomography scan (CT) showed a thick-walled cystic structure containing stones in the gallbladder fossa which was indicative of chronic inflammation (Figure 1). Subsequent magnetic resonance cholangiopancreatography (MRCP) displayed evidence of a remnant gallbladder containing a 6-mm calculus (Figure 2). Patient was then scheduled for an elective robotic-assisted laparoscopic cholecystectomy for removal of the remnant gallbladder.
In the operating room a Veress needle was used to induce pneumoperitoneum, and the abdomen was entered supra-umbilically under direct visualization via Optiview. Trochars were placed in standard fashion, and the robot was docked. The gallbladder was visualized and retracted superiorly. The area where the gallbladder joined the cystic duct was identified, and the fatty tissue surrounding the cystic duct was dissected away, which allowed for visualization of the cystic artery. This was similarly skeletonized and dissected free of fatty tissue. The gallbladder was then taken down from the gallbladder fossa on each edge using electrocautery. At this point, the critical view was obtained, the cystic duct and cystic artery were clipped with two clips on the proximal portion and subsequently divided. The remnant gallbladder was taken down off the gallbladder fossa using electrocautery and placed into a retrieval bag, which was taken out through the midclavicular incision.
The patient’s post-operative course was uneventful, and he was discharged on the same day as surgery. He reported no complications during follow-up visits.
Discussion
Subtotal cholecystectomies have been identified as accounting for between 4% to 9% of all cholecystectomies.3 The purpose of performing a SC is to prevent injury to the bile duct when the critical view of safety is unachievable. Rarely, the remaining section of gallbladder can contain calculi and develop symptoms. A study in 2009 found 4.19% of patients who underwent subtotal cholecystectomy developed symptomatic bile duct calculi.4 Another study identified cholecystitis developing in 1.6% of patients undergoing cholecystectomy.5 Completion cholecystectomies are rare, with only 0.32% of SC patients requiring one.6 In our case, the patient had a history of subtotal cholecystectomy combined with symptomatic cholelithiasis, which necessitated treatment with an elective completion cholecystectomy.
Remnant cholecystitis is caused by the same mechanisms that cause cholecystitis. Occlusion of the cystic duct or inadequate emptying of bile from the gallbladder can result in acute cholecystitis. Cystic duct obstruction is the most common etiology of acute cholecystitis, which is often caused by gallstones. Intermittent obstruction of the cystic duct by stones can cause biliary colic, which often presents as right upper quadrant (RUQ) pain.7 In contrast, acute cholecystitis is caused by persistent obstruction of the cystic duct, which results in inadequate drainage of bile from the gallbladder. Disruption in the draining of bile causes an increase in intraluminal pressure, which can lead to inflammation and potentially ischemia.8 Stagnant bile also provides an environment for bacterial colonization, which may contribute to the inflammation in acute cholecystitis.9 In our case, the patient’s remnant gallbladder segment contained gallstones, which eventually obstructed the cystic duct leading to acute cholecystitis. Cholecystitis can also develop without obstruction to the cystic duct. This often occurs in critically ill patients due to a variety of factors. Ischemia due to hypotension, vasoactive drugs, or surgery and trauma all prevent the gallbladder from normal emptying. Cholestasis can also be caused by prolonged fasting states, long term parenteral nutrition, and bowel obstruction.10 Similar to calculous cholecystitis, acalculous cholecystitis is a result of stagnant bile and increased intraluminal pressure.
Cases of remnant cholecystitis often present as persistent RUQ abdominal pain, nausea, and epigastric tenderness after initial subtotal cholecystectomy. Cases have also been reported of patients developing jaundice, cholangitis, fatigue, and chills.11,12 Murphy’s sign is a common indication of cholecystitis, which is inspiratory arrest during palpation of the RUQ.8 In our case, the patient presented with worsening RUQ pain tender to palpation, nausea, and decreased oral intake tolerance. However, he displayed a negative Murphy’s sign. Patients also may present with elevated inflammatory markers and hepatobiliary enzymes.11,12 In our case, the patient displayed an elevated white blood cell count with elevated lymphocytes and low neutrophils.
Physical examination and blood work narrow down the symptoms to hepatobiliary origin, but imaging allows for a definitive diagnosis to be made. If patients present to the emergency room, they may receive an abdominal CT scan as an initial study. This can display gallbladder dilation, gallbladder wall thickening, and radio-opaque stones.8,11,13 However, if cholecystitis is already suspected, an abdominal ultrasound may be used as a less expensive initial imaging study compared to CT scans. A study by Singh et al. demonstrated ultrasonography accurately identifying calculi in remnant gallbladders in 89% of their sample.14 However, in this study abdominal ultrasound failed to diagnose remnant gallbladder cholelithiasis in 11% of their patients. Similarly, Dikmen et al. displayed a failure to identify the remnant gallbladder in four (36.3%) of their eleven patients.12 The most definitive method of identifying the remnant gallbladder and surrounding anatomy is with an MRCP. In the study performed by Singh et al. MRCP was able to accurately diagnose remnant gallbladder calculi in all but two (4%) of the patients that underwent one.14 In our case, the patient presented to the emergency room initially, so he received a CT scan and an MRCP which led to the final diagnosis of remnant cholecystitis.
Treatments for remnant cholecystitis include endoscopic retrograde cholangiopancreatography (ERCP) and completion cholecystectomy. ERCP is only performed in certain cases where stones in the common bile duct are identified with imaging studies.14 It acts as both a treatment and a diagnostic tool, because it provides the opportunity to remove stones while visualizing the common bile duct. It does not directly treat cholecystitis but can treat complications such as cholangitis or choledocholithiasis, which patients with remnant gallbladders may encounter. The definitive treatment is completion cholecystectomy, which can either be performed laparoscopically or open. Most cases, like ours, describe the use of pre-operative antibiotics prior to completion cholecystectomy.11,13 Laparoscopic completion cholecystectomy is highly effective and had a success rate of 94.4% in a study done by Jebakumar et al.15 However, it must be performed by an experienced laparoscopic surgeon because of the need for extensive adhesiolysis and increased risk for bile duct injury. Utsunomiya et al. described two cases of laparoscopic completion cholecystectomy where adhesions between the gallbladder bed, hepatoduodenal ligament, and duodenum.16 In the second case of their report, the dissection at the border of the duodenum-like structure resulted in an injury to the bulb of the duodenum. Bowel injury, bleeding, and bile duct injuries are all potential complications of cholecystectomies in gallbladders with difficult anatomy. Iatrogenic injury of the bile duct can lead to bile leaking, which can lead to peritonitis and infection. Similarly, bowel injuries that lead to perforation can lead to peritonitis, sepsis, and multi-organ failure. Injury to the surrounding vasculature such as the right hepatic portal vein, cystic artery, and right hepatic artery can result in bleeding and hematoma formation.17 Some surgeons may feel more comfortable dissecting the adhesions in this area with an open approach. Completion cholecystectomy via laparotomy was described in Teshima et al., which resulted in one complete removal and one subtotal resection of the remnant gallbladder.11 However, in the repeated subtotal, they were able to remove the stones from the remnant gallbladder. Robotic laparoscopic surgery, like our case, has also been reported as a reliable method for completion cholecystectomy.18 In Gijsen et al they had no conversions to open and no vascular or bile duct injuries. However, unlike our case, these cases were fluoroscopy-guided using indocyanine green to visualize the extrahepatic structures intraoperatively. The robotic approach in our case allowed for careful dissection of surrounding fatty tissue and adequate view of the critical view of safety, thus preventing intraoperative complications allowing for an uncomplicated post-operative recovery. Regardless of surgical approach, completion cholecystectomy is an effective approach of treating remnant cholecystitis.11–16,18
Conclusion
Subtotal cholecystectomies are often performed for patients with complex anatomy within Calot’s triangle. Difficulty achieving the critical view of safety increases the risk of injuring the bile duct, which can lead to further complications. The subtotal cholecystectomy is a safe and effective method of mitigating risk of injuring the bile duct but comes with the risk of developing cholecystitis in the remnant gallbladder. Leftover stones in the remnant gallbladder can continue to cause persistent symptoms, which may require surgical intervention. Advancements in laparoscopic technique and the integration of robotic-assisted laparoscopic surgery has made completion cholecystectomies possible even in patients with complex anatomies. To minimize the risk of remnant cholecystitis, the surgeon should attempt to evacuate the gallbladder of as many stones as possible when performing a subtotal cholecystectomy.
_and_axial_(b)_ct_scan_of_stones_inside_the_remnant_gallbladder_with_surroundin.png)
_and_axial_(b)_ct_scan_of_stones_inside_the_remnant_gallbladder_with_surroundin.png)