Introduction
Renal cell carcinoma has spectrum of presentations. Paraneoplastic manifestations accounts for 10% of presentations. Hypercalcemia, hypertension, anemia, polycythemia, non-metastatic hepatic dysfunction (Stauffer’s syndrome), neuromyopathy and prostaglandin elevation are paraneoplastic manifestations described among RCC patients. Stauffer’s syndrome is a rare paraneoplastic hepatic dysfunction commonly associated with renal cell carcinoma (RCC), in the absence of hepatic metastasis. It often presents with abnormal liver function tests (LFTs), hepatosplenomegaly, and cholestatic jaundice.
Case Summary
A 29-year-old young female presented to emergency department (ED) with right sided abdominal pain and fever for 2 days duration. She denies any urinary symptoms, including hematuria and no sexual encounters. Initial examination Urine hCG was negative. She had an emergency laparotomy for ruptured ectopic pregnancy. She denies the history of jaundice, weight loss, alcohol use and hepatotoxic drug intake. On examination, she was alert and conscious with the Blood pressure of 90/60 mmHg. She is not pale or icteric. Abdominal examination revealed a ballotable right renal mass.
Initial basic investigations were performed and said to be normal. Liver function test (LFT) revealed alteration in enzymes and bilirubin levels, such as - AST -378, ALT – 366, GGT – 403, ALP – 433, Serum Albumin – 3.1 g/dL (3.5 - 5) and Total Bilirubin – 6.5 mg/dL (0.3 – 1.2) with direct fraction of 3.6 mg/dl. Serological tests for hepatitis B virus (HBV) and hepatitis C virus (HCV) were negative. Immunological assays for the various auto-immune diseases (ANA, anti-ssDNA, ASMA, p-ANCA and c-ANCA) were all negative. The urine analysis showed hematuria, blood and urine cultures were sterile. Ultrasound scan demonstrated large (10x6cm) heterogenous right renal mass suggestive of Angiomyolipoma and for further information, a contrast CT was performed. Computed tomography (CT) revealed 11x11x10 cm heterogeneously enhancing lesion arising from upper pole of right kidney suggestive of Renal cell carcinoma without any renal vein or inferior vena cava (IVC) thrombus and no paraaortic lymphadenopathies.
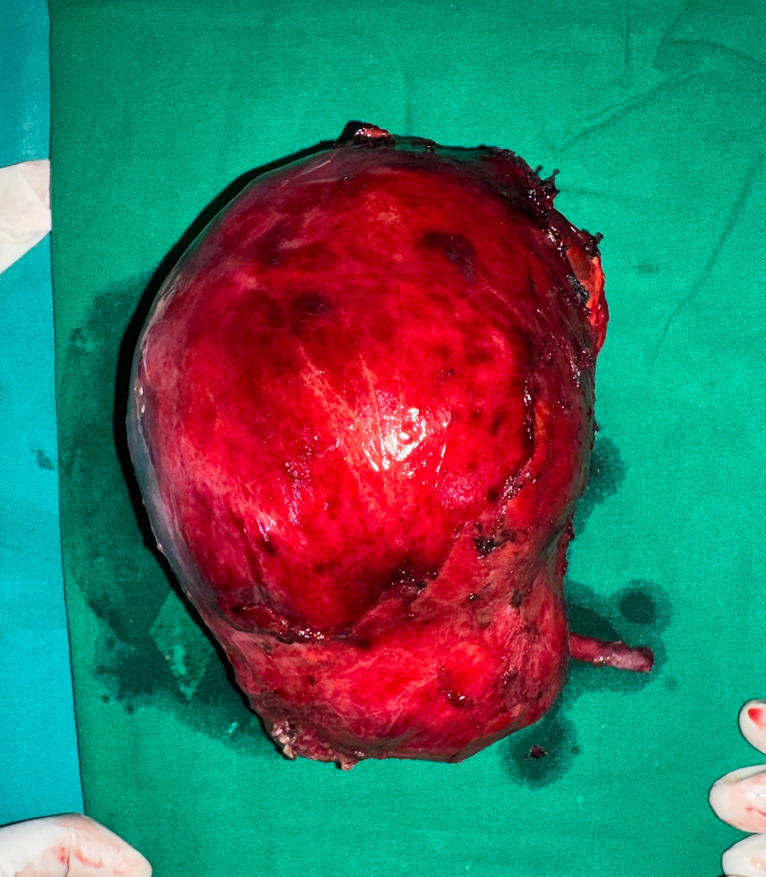
After anesthetic review and optimization, patient was counselled and taken for right Radical nephrectomy. Her post-operative recovery was uneventful and discharged on day 6. Post-nephrectomy histopathology revealed Clear cell RCC, Fuhrman grade II, confined to kidney with negative margins. A month after surgery, a full liver function test (LFT) was performed, and liver enzymes and bilirubin levels had returned to baseline, supporting a diagnosis of Stauffer’s syndrome.
Discussion
Cholestatic jaundice within the context of malignancy is usually associated with widespread hepatic metastasis or mechanical obstruction to bile flow.1 Stauffer’s syndrome is a rare but recognized paraneoplastic manifestation of RCC, typically characterized by; Abnormal liver enzymes (especially ALP and GGT), hepato-splenomegaly, absence of hepatic metastasis and complete resolution of clinical and liver function abnormalities.
The underlying pathophysiology of this paraneoplastic manifestation is poorly understood. Nevertheless, this syndrome is thought to be mediated by inflammatory cytokines, especially interleukin-6 (IL-6), which alters hepatic metabolism and cholestasis. This results in cholestatic liver enzyme patterns without histological evidence of liver disease. A few studies have shown that patients with metastatic renal cell carcinoma with detectable IL-6 had significantly higher serum ALP and GGT levels,2 this further support the role of IL-6.
The diagnosis is one of exclusion, requiring the elimination of viral, autoimmune, and structural causes of liver dysfunction. In this case, comprehensive liver workup was negative, and imaging ruled out metastases. The dramatic resolution of liver enzymes post-nephrectomy confirms the paraneoplastic nature. Stauffer’s syndrome may precede the diagnosis of RCC and should be considered in unexplained hepatic enzyme elevations, particularly with systemic symptoms like weight loss or fatigue.
Conclusion
This case underscores the importance of considering Stauffer’s syndrome in the differential diagnosis of unexplained hepatic dysfunction, even in the absence of typical RCC symptoms.
Early detection of RCC through such atypical presentations allows timely intervention, often curative. Awareness of this paraneoplastic phenomenon among clinicians and surgeons is essential for improved diagnostic accuracy and patient outcomes.