Introduction
The presence of malignant tumors within the contents of hernia sacs, or metastatic implants in the sac wall, is uncommon, with very few cases reported in the surgical literature. Arnaud described the first case in 1749, and Lejars in 1899 classified hernia tumors as sacular (originating from the sac itself) or intrasacular (arising from organs contained within the sac).1,2
Roslyn reviewed 23 cases of hernia tumors in 1980, reporting 7 sacular and 16 intrasacular tumors, of which 7 were colonic carcinomas.3 Later, Pappas et al. found 12 cases of inguinal hernia containing colon cancer, predominantly involving the sigmoid colon.4
The incidence of colon carcinoma within inguinal hernias ranges between 0.03% and 0.5%.5 In general, clinical suspicion arises when a long-standing hernia becomes irreducible, enlarges rapidly, or is associated with gastrointestinal symptoms. Despite this, up to 50% of diagnoses are made intraoperatively, leading to incomplete staging and challenging management.6
This case report contributes to the scarce literature on this rare condition and highlights the importance of considering colonic malignancy in elderly men presenting with irreducible inguinoscrotal hernias.
Case Summary
A 77-year-old male with a past medical history of systemic hypertension controlled with losartan, and deep venous thrombosis of the left leg 10 years prior without treatment, presented with a right inguinal mass of 10 years’ progression and growth. Eight years later, he developed contralateral growth that limited daily activities. He attended the outpatient clinic 8 months prior, where he was diagnosed with bilateral inguinal hernia and scheduled for elective surgery in March 2024.
On physical exam: globose abdomen secondary to adiposity, soft, depressible, non-tender. Left inguinoscrotal hernia (20 × 10 cm in size), right inguinoscrotal hernia (20 × 15 cm in size), non-transilluminating, non-reducible, palpable hernia rings, no skin changes or tenderness, peristalsis present in the scrotum.
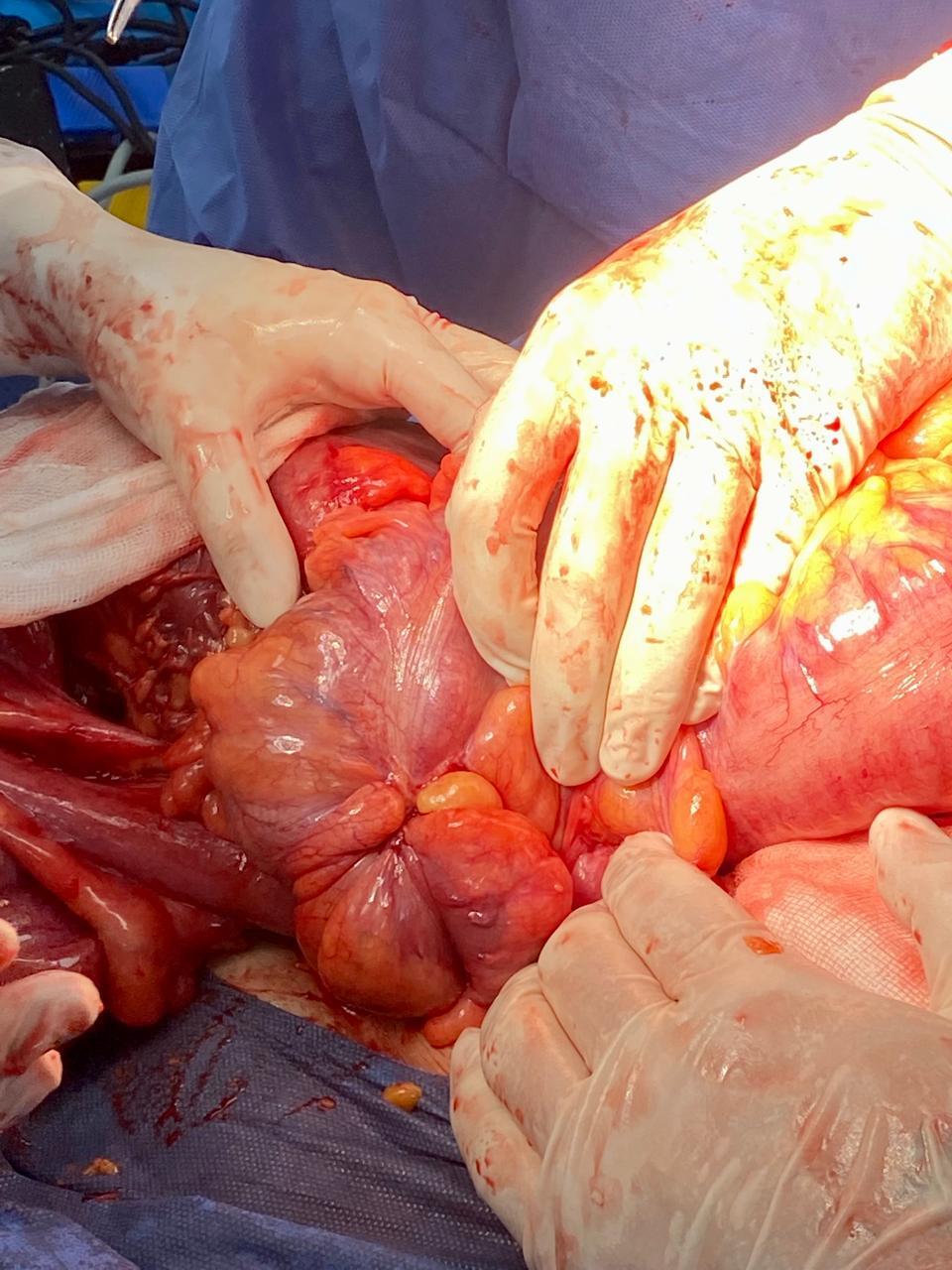
He was taken to the operating room for elective repair. Under general anesthesia with endotracheal intubation, a midline supra- and infra-umbilical laparotomy was performed. On exploration, reactive fluid was found, with a dilated bilateral deep inguinal ring of 7 cm. Herniated bowel loops were reduced, revealing a volvulus of the ascending colon on the right side (Figure 1) and a sigmoid colon mass within the left inguinal canal (Figure 2). The entire colon was dilated (>10 cm) with wall involvement.
Catell and Mattox maneuvers were performed, with safe mobilization of the hepatic and splenic flexures. Vessels were identified (ileocolic, right colic, middle colic, left colic, and sigmoid arteries). Resection was performed from the terminal ileum (30 cm from the ileocecal valve) to 10 cm proximal to the rectosigmoid mass, preserving the rectum. The distal stump was closed in two layers (continuous 3-0 vicryl suture, then 2-0 silk Lembert sutures). A terminal ileostomy was matured using Brooke’s technique. Hemostasis was confirmed, drains were placed, and closure was performed.
The surgical specimen measured 204 cm of colon with a circumference up to 26 cm. Gross pathology showed a distal lesion, 7 × 5 × 1.5 cm, partially occluding the lumen, with a rough white surface, semi-firm, located 5 cm from the distal margin. The appendix measured 3.5 × 0.5 cm, grossly normal. Histopathology reported a moderately differentiated invasive adenocarcinoma, ulcerated, infiltrating up to the muscular wall and pericolic adipose tissue.
Postoperatively, the patient developed acute-on-chronic renal failure, metabolic acidosis, and respiratory distress requiring airway management. He suffered hemodynamic collapse and cardiac arrest. Despite resuscitation efforts, the patient died.
Discussion
This case illustrates the rare coexistence of bilateral giant inguinoscrotal hernias with colonic adenocarcinoma. Most reported cases occur in elderly men and involve the sigmoid colon, which is consistent with our findings.4,5
According to Lejars’ classification, the tumor described here corresponds to an intrasacular tumor, originating from a primary neoplasm of an organ within the hernia sac.2 While metastatic disease to the hernia sac is more common, primary colonic carcinoma within a hernia is extremely rare.7
Diagnostic imaging, particularly CT scanning, is considered the most effective tool to identify both the hernia contents and possible underlying malignancy.8 Unfortunately, many cases—such as this one—are diagnosed intraoperatively, limiting the opportunity for preoperative staging.
Management remains controversial. Some authors advocate for a single inguinal approach when feasible, though this risks inadequate oncologic resection. Laparotomy provides better exposure for colonic mobilization and staging.9 Hernia repair in the presence of colonic resection is debated: prosthetic mesh is generally avoided due to infection risk, and herniorrhaphy is often preferred, albeit with a higher recurrence rate.10
Prognosis depends largely on tumor stage and comorbidities. Reported mortality remains high, particularly in emergencies or advanced presentations.6 Our patient unfortunately developed postoperative complications culminating in death, underscoring the fragility of this population.
Conclusion
Inguinal hernias containing colonic carcinoma are rare but clinically significant. Surgeons should maintain suspicion in elderly patients with long-standing, irreducible, or atypical hernias. Early imaging and multidisciplinary management may improve diagnostic accuracy and outcomes.
Treatment discussions focus on the surgical approach and hernia repair strategy in the presence of tumor mass and megacolon with colonic wall involvement. Approaches may be inguinal or abdominal. The inguinal approach allows simultaneous treatment of both diseases and avoids laparotomy but requires wide oncologic resection. Its disadvantage is surgical site infection, since the operation involves both a clean (hernia repair) and a clean-contaminated (colon resection) procedure. In such cases, herniorrhaphy is preferred over mesh hernioplasty due to lower infection risk, despite higher recurrence.
In our case, colectomy with terminal ileostomy was performed due to the involvement of the entire colon, with the expectation of managing postoperative electrolyte disturbances and motility disorders.