Introduction
Pseudoaneurysm of the superficial temporal artery (STA) is rarely encountered, generally occurring after blunt trauma located in the frontotemporal region.1 Literature indicates that this type of pseudoaneurysm (PSA) may also develop following penetrating trauma or surgical intervention, such as craniotomy. These pseudoaneurysms tend to exhibit progressive growth, and if left untreated can eventually lead to severe hemorrhage.2 They commonly present as either a subtle subcutaneous lump or a large, pulsatile mass with a potential for significant bleeding.3 Many patients may remain asymptomatic aside from noticeable cosmetic deformities, while others may experience headaches, facial pain, or facial nerve palsy due to proximity of the facial nerve in this region.4 In this report, we present a case of a PSA of the STA resulting from a mechanical fall.
Case Summary
An 85-year-old patient with a past medical history significant for hypertension, anticoagulated for atrial fibrillation, Parkinson’s disease, presented to our emergency department after a mechanical fall sustaining a left forehead laceration, which was repaired with non-absorbable sutures. All trauma work-up was negative for any acute traumatic injury, and patient was discharged to home. At a follow-up outpatient clinic visit a week later he was noted to have a hematoma on the left forehead/parietal area, but otherwise the wound was healing well. Sutures were removed, and there was no active bleeding noted at that time.
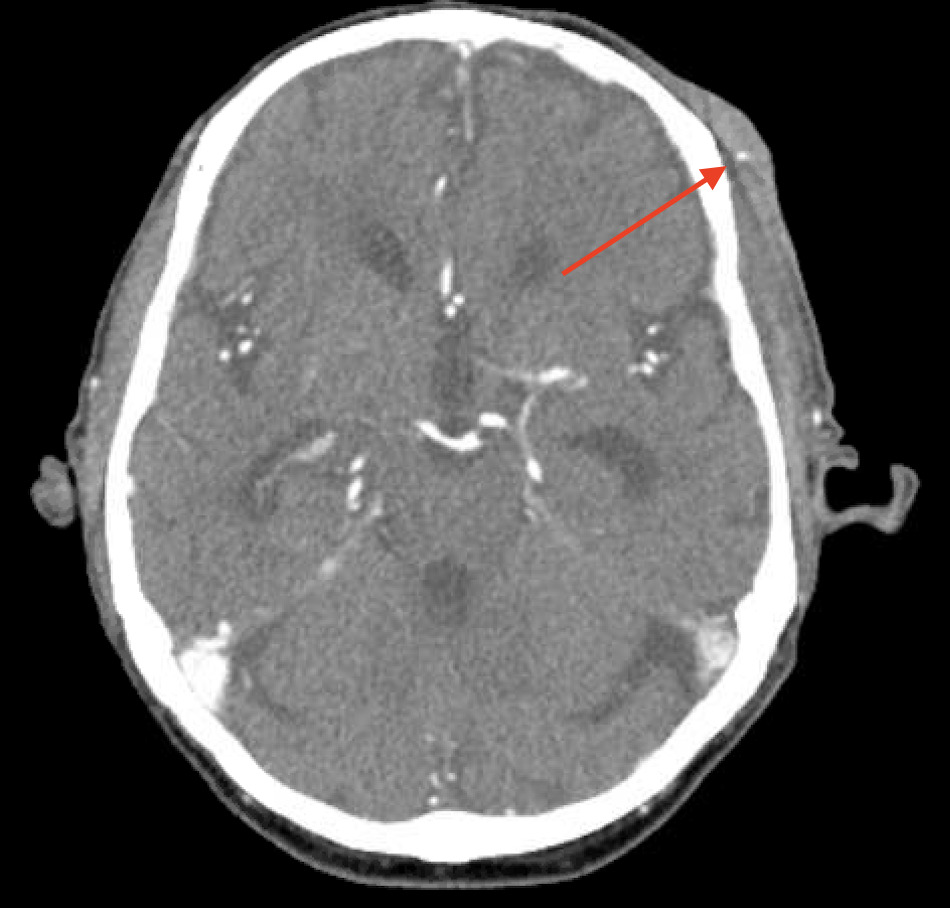
Patient presented to our emergency department 14 days after the initial trauma with oozing and concerns of worsening hematoma on the left forehead (Figure 1). His wound was dehisced, with old clots within the wound bed. At this time patient was mainly complaining of mild headaches. He remained hemodynamically stable. Upon evaluation the wound was irrigated, and clots were carefully removed. There was no active bleeding noted but a pulsatile vessel was easily palpable at the inferior portion of the wound bed. Ultrasound was obtained and showed an 0.8-cm hematoma with a pseudoaneurysm (Figure 2). A CT angiogram of the head and neck confirmed a 6-mm PSA of the left STA in proximity with the left frontal scalp hematoma (Figure 3). Patient underwent a coil embolization of the anterior division of the STA which was the main vessel feeding the PSA (7x3mm) (Figure 4). Patient had no further bleeding and was discharged to home the following day. He is progressing well, with no further post-operative complications.
Discussion
Our report highlights the importance of maintaining a high index of suspicion for a pseudoaneurysm (PSA) after a head trauma. Although hematomas and PSAs of the superficial temporal artery (STA) often present similarly, a key distinguishing feature of a PSA is the presence of a pulsatile mass, which may sometimes be associated with active arterial bleeding, suggesting that the mass could be related to either an aneurysm or a PSA. When a PSA is suspected, the recommended initial diagnostic test is a Doppler ultrasound, followed by CT angiography, MR angiography, or conventional angiography. The primary goal of PSA treatment is to prevent rupture and subsequent hemorrhage. Surgical ligation and resection remain the most effective standard treatment,1,5 involving the exclusion of both afferent and efferent vessels along with excision of the PSA. Alternative treatment options include ultrasound-guided thrombin injection and endovascular coil embolization. In cases of hemodynamic instability, emergency surgery is warranted. If surgical removal poses significant challenges, endovascular treatment should be considered. If left untreated, a PSA may rupture, leading to life-threatening hemorrhage, and achieving hemostasis can be difficult. Therefore, early diagnosis and intervention are essential.
The most common etiology of PSAs remains blunt or penetrating trauma. It is believed that the STA is particularly susceptible to injury and PSA formation during impacts due to the absence of a muscular cushion that protects the artery from the underlying temporal bone. Notably, regression of a PSA after coil embolization has been documented,5 with a 12-month follow-up indicating complete obliteration of the pseudoaneurysm and no cosmetic repercussions. The case we are presenting is a patient with multiple comorbidities, with no active bleeding on examination, and a clean wound bed, therefore a decision was made to proceed with coil embolization. This approach resulted in excellent hemostasis and minimal intraoperative blood loss.
It remains essential to conduct a thorough evaluation of each patient prior to making any decisions regarding the treatment plan. In case of active hemorrhage, hemodynamic instability or expanding hematoma, the preferred or standard treatment is surgical exploration, including ligation of the afferent and efferent vessels supplying the pseudoaneurysm.
Conclusion
Undiagnosed traumatic pseudoaneurysms of the superficial temporal artery can lead to life threatening hemorrhage. Therefore, it is very important to maintain a high clinical index of suspicion when evaluating patient with trauma of the frontotemporal region. While endovascular interventions can be successful in non-bleeding pseudoaneurysms of the superficial temporal artery, surgical exploration is recommended in the presence of active hemorrhage, hemodynamic instability, or expanding hematoma.



_coil_embolization_of_the_anterior_division_of_the_sta_which_was_the_main_vessel_feedin.png)


_coil_embolization_of_the_anterior_division_of_the_sta_which_was_the_main_vessel_feedin.png)